Introduction:-
This is a new investigation in vestibulometry and a very useful addition to the neurotologist’s diagnostic armamentarium. It evaluates the functional status of the rotational vestibulo-ocular reflex (rVOR) of the six semicircular canals at high frequencies of vestibular stimulation. The term rVOR refers to the biological mechanism by which the visual surroundings appear stable to us when we rotate our heads at a high speed in the horizontal or vertical planes. Maintaining a stable image of the visual surroundings (termed as ‘gaze stabilization’ in medical parlance) is one of the primary functions of the vestibular system and the maintenance of gaze stabilization on rapid rotation (fast angular movement) of the head is the specific function of the semicircular canals in the inner ear. If the semicircular canals are defective, the rVOR is jeopardized. Hence, one of the best ways to assess the functional status of the six semicircular canals is to evaluate the efficacy of the rVOR of the six different canals and ascertain whether the rVOR is capable of stabilizing images of the visual surroundings when there is a fast head movement. The fHIT precisely does that. i.e., assesses whether the rVOR of the semicircular canals are being able to stabilize images when there is a fast head movement in the plane of the semicircular canals. In persons with a defective rVOR, whenever the head is rotated rapidly in any direction, the images of the visual surroundings are not stable / fixed in the eye leading to
- A blurring of the visual surroundings,
- A loss of visual acuity
and - A sense of head spinning.
There are many tests to evaluate the six semicircular canals like the caloric test VNG/ENG, the Dynamic Visual Acuity (DVA) test, the newly introduced Gaze Stabilisation Test (GST), the Video Head Impulse Test (VHIT) etc. So what is so very special in the Functional Head Impulse Test (fHIT), and do we really need a new test?
The relevance of fHIT in contemporary Vestibulometry:-
The USP of fHIT is that this is a functional test and reliably measures the functional status of the semicircular canals (by ascertaining the efficiency of the rVOR) in a quick, very simple, easy to perform way without much of complicated, cumbersome and costly equipment that is necessary for the other tests. It does not ascertain the VOR gain which the VHIT does, or measure the percentage of canal paresis that the caloric test ENG / VNG does, or even measure the loss of visual acuity that the DVA test does, but it assesses whether the semicircular canals are being able to serve the function of gaze stabilization and, if so, how efficiently. This qualitative rather than quantitative measurement is a more practical approach and more relevant to the clinician as all that the clinical practitioner in neurotology is interested to know is whether the semicircular canals are serving their function of maintaining a stable gaze when there is a fast head movement. In fact, in the clinical practice of neurotology, the functional status of an organ is much more appropriate as a clinical parameter than mathematical values like the % of canal paresis (that is measured by caloric ENG/VNG) or the % of the VOR gain (measured by the VHIT) of the semicircular canals. Of course, the qualitative evaluation obtained by fHIT can be documented quantitively also as detailed later.
The physiological mechanism tested by fHIT vis a vis the other tests:-
The fHIT ascertains the efficiency of the semicircular canals in stabilizing images in the eyes so that when we move (rather, rotate) our heads in different directions, the visual surroundings appear stable and there is no loss of visual acuity. Visual acuity (VA) is defined as the clarity of vision and is dependent primarily on the sharpness of the retinal focus within the eye. If the visual surroundings are not stable there will naturally be a loss of visual acuity. It is much easier for us to read a sign post in the road when the car is stationary rather than when the car is moving very fast. This stabilization of the image of the surroundings which gives us the sharpness of retinal focus is effected by the rVOR generated by the semicircular canals. When there is a sudden movement / rotation of the head, the vestibulo-ocular reflex brings about a movement of the eyes at a speed that is equal to the speed of the head movement but in the opposite direction to that of the head movement. This ensures that images of the visual surroundings remain fixed in the fovea, which is the most sensitive part of the retina no matter how fast we rotate the head. If the head is rotated at a speed of 200 degrees /sec to the left then the generated rVOR makes the eyes move to the rightat a speed of 200 degrees /sec. in a normal person. If the head moves upwards at 200degrees/sec then the eyes will automatically move downwards at 200degrees/sec. This ensures perfect gaze stabilization. The ratio of the speed of eye movement to that of the head movement is the ‘gain’ of theVOR. When both speeds are equal then the gain of the VOR so generated is 100%, which is normal. If the semicircular canals are defective then the requisite speed of eye movement is not generated and the eyes may move at a speed of (say) 100 degrees /sec to the right when the head is moved at 200 degrees /sec to the left. In such a case, the gain of the VOR is 100/200 i.e. 50%. If the VOR is poor, then the requisite speed of eye movement is not generated and images of the visual surroundings slip out of the fovea thereby causing a loss of the sharpness of the visual focus. This causes a blurring of vision and a loss of visual acuity.Even a 2degrees slippage of the image from the fovea reduces the visual acuity by more than 50%. In the fHIT this degradation of visual acuity, if any, on sudden and fast head movement is evaluated. In the DVA test also, the status of the VOR (and indirectly that of the relevant semicircular canals also) is ascertained by assessing the degradation of the visual acuity on fast head movement. However, there is a difference in the process of computing the degradation of visual acuity in fHIT and DVAT which is elaborated later; in VHIT the degradation of visual acuity is not calculated but the gain of the VOR is calculated. In DVA we measure how much is the degradation of the Visual Acuity (VA) on fast head movement and if the loss of VA is more than 0.2logMAR (the unit by which VA is measured) then the VOR is considered subnormal which indicates a poor semicircular canal function. In VHIT it is the impairment of VOR gain (not the loss of VA) on fast head movement that is calculated. Since VHIT measures the gain of the VOR generated by the head movement, it requires a mechanism to measure the speed of the head movement as well as a mechanism to measure the speed of the eye movement. Measurement of the speed of head movement is technically a very easy process as gyroscopes and accelerometers are easily available which are very cheap but can very accurately monitor the direction and speed of head movement; however,measurement of eye movement is technically difficult and requires sophisticated high speed cameras and very complex computation. This makes VHIT a costly gadget that many practitioners find difficult to afford. Moreover, the more complex a gadget, the more it is susceptible to damage and prone to require service which is not always easy (rather impossible) to get in most places.
A very logical question that may arise in the reader’s mind (especially those who are yet to be neurotologically initiated), is why are we always stressing about fast head movements? The vestibulo-ocular reflex (VOR) brings about the process of gaze stabilization only when there is a fast head movement and not when there is a slow head movement; during slow head movement the gaze stabilization is carried out by the oculomotor system (specifically the smooth tracking system) without any involvement of the semi-circular canals. Hence, to evaluate semicircular canal function the rVOR needs to be generated, and this occurs only when the head movement is very fast.
As mentioned several times before, the function of the VOR is to keep visual objects in sharp focus and stable in the retina and thereby maintain a perfect visual acuity when there is a fast head movement. If the visual acuity is imperfect, there is a loss in the clarity of vision and hence a degradation in the subject’s capacity of clearly identifying an object. Hence, a poor rVOR would lower the subject’s capacity of clearly recognising a visual object whenever there is a fast head movement. So, the subject’s ability of correctly identifying a visual image (called ‘optotype’ in medical parlance) would be impaired whenever there is a fast head movement. This is exactly what is tested by the fHIT. In fHIT, the loss of visual acuity on fast head movement is evaluated by ascertaining whether there is a perceptible degradation in the subject’s reading ability which is bound to happen whenever the sharpness of the retinal focus is lost. If fast head movement cannot generate the requisite speed of eye movement in the opposite direction, then there will be a loss / degradation of visual acuity and consequently an impairment of readability. The fHIT ascertains this specific function i.e. whether there is a loss of the subject’s ability to correctly identify an optotype of a predetermined size (based on the subject’s visual acuity) when there is a fast head movement. It does not calculate the quantity of the loss of Visual Acuity in logMAR as in DVA which requires testing VA with gradually smaller size of optotypes. This process requires quite a bit of time and increases the complexity of the test; fHIT just determines whether there is any loss of readability of a pre-determined fixed size optotype on sudden head movement.Gradual reduction of the size of the optotypes is not required in fHIT. The size of the optotypes during the actual functional head impulse test (fHIT) is calculated by the fHIT system’s software and is 0.2 logMAR bigger than the lowest size of optotypes that the subject can correctly identify from a distance of 1.5 meters (called static visual acuity) when there is no head movement. As the fHIT does not calculate the VOR gain there is no need to measure the speed of eye movement. This simplifies the test in a very big way and bypasses the very complex process of documenting and calculating the speed of eye movement that requires extremely complex gadgetry and computation. But fHIT does very reliably tell us the functionality / efficacy of the generated VOR and that is all that the clinician needs.
So, fHIT is more like the DVA test but is even simpler than and without some of the shortcomings of the DVA test. The fHIT can test not only the lateral canals but also the vertical canals i.e., the anterior and posterior canals of both sides just like the VHIT. In DVA only the lateral canals are tested effectively not the vertical canals. In the caloric test VNG/ ENG also, it is only the lateral canals and not the vertical canals that are tested. fHIT serves the same purpose as the DVA and the VHIT as all of them test the rVOR to evaluate the status of the semicircular canals but fHIT does it in a much simpler, faster and more importantly in an inexpensive non-cumbersome way. Moreover, fHIT can evaluate the semicircular canal function at speeds much higher than that can be tested by DVA or by VHIT. fHIT objectively documents the performance of the patient’s VOR in real life practical situation and is tested with a physiological stimulus (i.e., fast head movement which we always do in our day to day lives) unlike the un-physiological stimulus (hot & cold stimulation) used in the caloric test. The instrumentation in fHIT is very very simple and involves just a small 2inch by 2 inch by 1/4th inch sized three axis gyroscope and accelerometer that is attached to a elastic head band and a small calculator type of patient response device. The footprint is negligible and requires one-half the space of that of a smart phone.

Fig1: The hardware of the fHIT system. The device is connected to an ordinary computer (not the very high end ones) through a USB port.
In clinical practice we need gadgets that are
- Easy to operate,
- Easy to acquire (i.e., cheap and affordable by private practitioners),
- Easy to maintain,
- Easy to handle and carry (as most practioners shuttle between clinics and also need to use them at the patient’s bedside),
- Generates easy to interpret results,
but at the same time evaluates the physiological function tested very reliably.
The advantage of fHIT is that it complies with all of the above. The methodology of the test is such that there are no false positive data i.e., no spurious data or artefacts generated by the device. An online feedback system constantly updates the operator on the exactness of test process.
The fHIT device and test process:-
The test is very simple to perform and can be very reliably done even by a trained assistant when the doctor is hard-pressed for time. This is a very big advantage in clinical practice especially in small private clinic set-ups.
The instrument has a 3 axis gyroscope and an accelerometer; the gyroscope can measure the rate of rotation around a particular axis. A three-axis gyroscope measures rotation in the X, Y and Z axes. The accelerometer is an electromechanical device used to measure acceleration forces and can gauge the orientation of a stationary item. Both (gyroscope+accelerometer) together can sense any head movement in any direction and calculate the speed and direction of the movement very accurately. All our smart phones are equipped with these devices (also called magnetometers), which are very small in size, very hardy (they hardly everconk off) and due to their very wide usage are available at very low prices.


Fig2 (A & B): The 3 axis gyroscope and an accelerometer housed in a small box (2A) attached to the elastic headband that the patient wears (2B)
The fHIT hardware consists of the above-mentioned device housed in a small box attached to an elastic head band (Fig1) that the patient wears (Fig2). The device is connected to a computer where the proprietary fHIT software is loaded. The patient is given a small hand held device that looks like a calculator and smaller than a mobile phone, which is the patient response unit. The unit has the 8 different type of Landolt Cs as shown in Fig 3.

Fig 3A: The patient response unit. This calculator shaped device has the eight types of Landolt ‘C’s which are the replicas of the optotypes that appear on the computer screen. The patient has to press the key that corresponds to the optotype appearing on the screen.

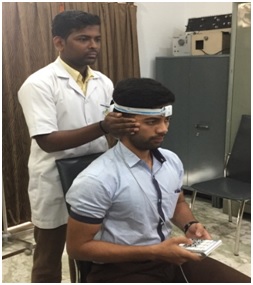
Fig 3B&C: The setup for the test at Vertigo & Deafness Clinic Kolkata India.The patient is seated 1.5 meters from the computer screen and holds the patient response unit in his hand. During the static VA test, the head is kept still and the VA is determined. Once the actual test starts the optotypes (the Landolt ‘C’s) appear briefly on the computer screen only when the patient is rotating the head fast enough (acceleration between 3000 to 7000 degrees/sec2 during the tests for the horizontal canals and between 2000 to 5000degrees/sec2 during the tests for the vertical canals) and in the correct plane. The optotype appears on the computer screen only during the phase of acceleration i.e., only for the very brief period when the speed of head movement is increasing and disappears when the speed of head rotation is fixed. Acceleration in physics is defined as the rate of change of speed; the semicircular canals can only be stimulated by acceleration i.e., only when the speed of head movement is changing. So the readability is tested only during the period of acceleration. As soon as the change of speed ceases, the optotype disappears from the screen. The patient has to perfectly identify the optotypes and press the corresponding key in the hand held patient response unit. The calculations like how many of the optotypes the patient is being able to correctly identify in different accelerations of head rotation is automatically done by the fHIT machine’s software.
The patient is made to sit about 1.5 meters away from the computer screen. To start the test, the static visual acuity (i.e., the VA with the head still) is first determined by asking the patient to identify Landolt ‘C’s of gradually smaller sizes till the patient cannot identify the optotypes correctly.This first step of determination of static visual acuity may be skipped for persons with normal eyesight but is necessary for persons with refraction errors. If the operator is not sure of the patient’s eyesight and in patients wearing spectacles, it is best to perform the static visual acuity test.For patents with spectacles the test can be done with the patient wearing the spectacles too.
Once this is done, the software automatically determines the fixed size of the optotypes at which the test will be done. The size of the test optotype is 0.2 logMAR units bigger than the static visual acuity of the patient.
After this, the proper test begins.A small dot appears on the computer screen and the patient is asked to visually focus on the dot at the center of the computer screen. The operator then selects the canal set to be tested viz. the lateral canals (left and rightlateral canals) or the right anterior canal and left posterior canal set (RALP) or the left anterior and right posterior canal set (LARP). Then the operator stands behind the patient (fig3B&C) and carries out the fast head movements correctly and very precisely in the plane selected canals (i.e., laterals/ RALP/ LARP). This is very easy and can be mastered by anybody with a 10-15 minute of training. The software of the fHIT system also monitors the plane of head movement and assists the operator in selecting the correct plane of head movement. The speed at which the operator moved the head (say, at a speed of 4275 degrees /sec)is visible to the operator on the computer screen.When the operator moves the head rapidly in the correct plane and within the specified speed limits, the Landolt ‘C’ appears in the computer screen as shown in Fig 4. The optotypes is there in the computer screen for a very brief period and only when the head is being rotated at an increasing speed (i.e., only during the phase of acceleration). The patient is asked to identify the opotype and press the corresponding key in the hand held device. The computer software keeps a count of the correct identifications at different speeds of head movements.
Fig 4: The patient has to identify the optotypes correctly and press the identical key in the hand held device.
 Fig 5: The patient responds by pressing the identical key in the hand held device.
Fig 5: The patient responds by pressing the identical key in the hand held device.

Fig 6: The test for the Right anterior and left posterior canals (RALP) being done. The operator stands behind the patient and rotates the head vertically in the plane of the right anterior and left posterior canals at a high speed.

Fig 7: The fHIT for the left anterior and right posterior canals (LARP) being done.
The operator is expected to move the head about 5 to10 times at speed ranges of 2000 to 3000 degrees/sec, 3000 to 4000 degrees/sec,4000 to 5000 degrees/sec, 5000 to 6000 degrees/sec. The number of correctly identified optotypes (the Landolt ‘C’) in each of the speed ranges is depicted as bar graphs for each of the speed ranges (like 3000 to 4000 degrees/sec2 , 4000 to 5000 degrees/sec2) called ‘acceleration bins’ with the age and sex corrected normal ranges superimposed for comparison. The outcome of the test is the percentage of correct optotype identifications at different head accelerations.
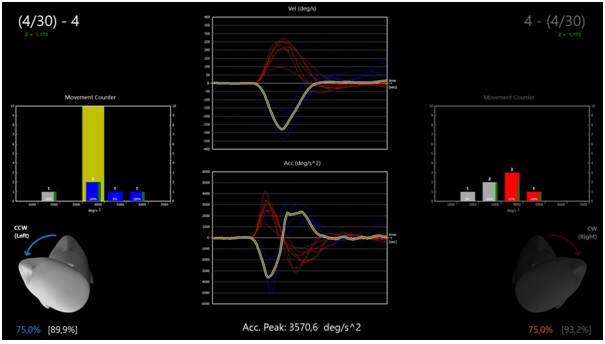
Fig 8: While the test is being done, the operator can constantly monitor the acceleration and velocity graphically as well as the number of times the test has been done at each range (accelaration bin). The movement highlighted in yellow is the last movement made. In the above figure, the yellow marked one is a test for the left posterior canal. The left sided tests are marked in blue and the tests on the right canals (lateral / anterior/ posterior) in red.
The results and the interpretation:
The results are presented synoptically in the form of bar graphs separated for each acceleration range. Hence, the clinician can know at which particular range of acceleration of head movement is the rVOR deficient in which particular canal i.e., which semicircular canal is performing sub-normally at which frequency of vestibular stimulation. This is very important as the physical therapy for correction of the deficit has to be customized accordingly. The system also an added physical therapy unit by which the canals can be stimulated at different frequency ranges. The fHIT assesses the semicircular canal function over a range of frequencies very much like the VHIT, but at a wider range of frequencies than the VHIT. In the DVA though the stimulation of the lateral canals are done at different frequencies, yet the results of the DVA do not show the frequencies (or the acceleration of head movement) of vestibular stimulation.The range of accelerations are also much lesser in DVA than that of the fHIT.
Fig 9: The printout obtained from the machine shows the results of the tests for the lateral canals (upper left box), the RALP (upper right box) and LARP (lower left box).
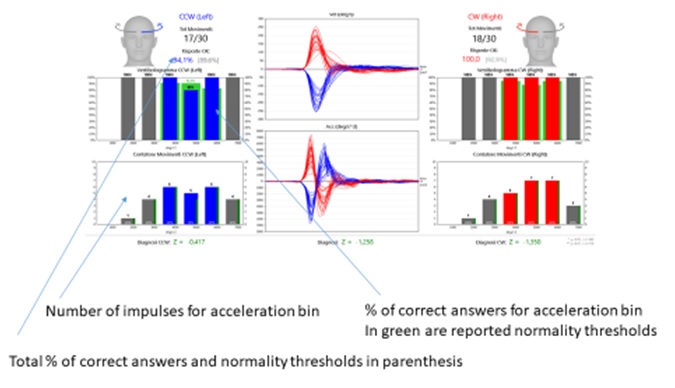
Fig 9A: The two bar charts on each side graphically depict the test. The upper two are called the vestibulograms of the left (in blue) and the right canals (in red). The lower two are the number of head movements done in each acceleration bin.These lower boxes are called the movement counters so that the clinician can know how many head movements were done in each of the acceleration bins. Ideally, there should be about ten movements in each of the acceleration bins for both sides i.e., ten fast head movements between 3000 to 4000 degrees/sec2 ,ten fast head movements between 4000 to 5000 degrees/sec2 ,ten fast head movements between 5000 to 6000 degrees/sec2.
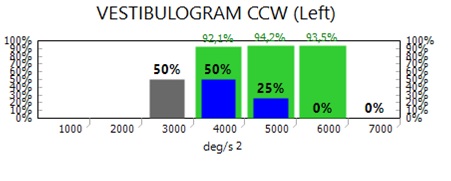 Fig 9B: A closer look of the vestibulogram. This is a vestibulogram of one of the canals of the left side(as indicated by the blue colour of the bar graphs). It also indicates that between 3000 to 4000degrees per sec2acceleration there were only 50% correct responses whereas the age–sex matched normal range for this acceleration bin is 92.1% ; also between 4000 to 5000degrees per sec2 acceleration there were only 25% correct responses whereas the age–sex matched normal range for this acceleration bin is 94.7%.
Fig 9B: A closer look of the vestibulogram. This is a vestibulogram of one of the canals of the left side(as indicated by the blue colour of the bar graphs). It also indicates that between 3000 to 4000degrees per sec2acceleration there were only 50% correct responses whereas the age–sex matched normal range for this acceleration bin is 92.1% ; also between 4000 to 5000degrees per sec2 acceleration there were only 25% correct responses whereas the age–sex matched normal range for this acceleration bin is 94.7%.
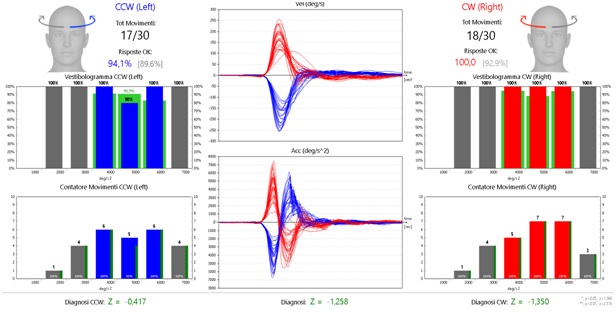
Fig 10: The results of fHIT of the lateral canals in a healthy subject. The grey bars represent data that are out of the interesting range for diagnosis, which is considered to be, for lateral test, from 3000 to 6000 deg/sec2.. The blue bars are the results for the left side (left lateral canal) and the red bars are the results for the right lateral canal. The green bars on which the blue and red bars have been superimposed are the age and sex matched normal ranges.
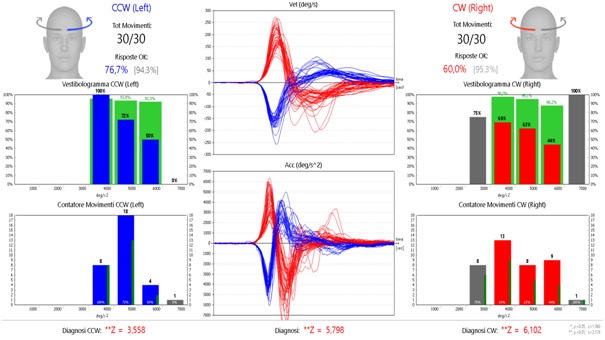
Fig 11: The fHIT results in a patient of bilateral lateral canal deficit. On the left side the response as plotted in the vestibulogram is subnormal only at high frequencies i.e., at accelerations of 3000 to 4000 degrees/sec2 and worse at 4000 to 5000degrees/sec2. The test has not been done at 6000 to 7000degrees /sec2 acceleration. On the right, the vestibulogram for the right lateral canal shows poor rVOR at all the three acceleration bins as the green bars which depict the age-sex matched normal values are much higher than the red bars which depict the percentage of correct responses (i.e., correctly identified optotypes) for the right lateral canal in the different acceleration bins.
Conclusion:
The fHIT is hence a very useful addition to the neurotologist’s diagnostic armamentarium and a boon to the clinician in many ways. We have been using the system in our clinic for the last two weeks and it has been a fascinating experience. The engineer who had devised the machine had flown down from Italy and was with us for a couple of days for clinical evaluation. We have picked up quite a few cases of abnormalities by fHIT especially in the high frequency range where the patient had balance problems but all the other tests have shown normal findings.
The best part is the added special semicircular canal rehabilitation program (physical therapy) whereby the defective semicircular canals can be stimulated at different accelerations depending on the range (acceleration bin) where the abnormality has been found. The software for the rehabilitation program can be loaded into the patient’s smart phone and a small patented sensor given to the patient so that the rehab can be carried out by the patient at home also. This rehabilitation part will be elaborated in a later communication.