Introduction:
Disorders of the balance system that includes vertigo/imbalance/dizziness affect a huge portion of the population. Prevalence is 1.8% in young adults and more than 30% in the elderly. 65% of individuals older than 60 years of age experience dizziness or loss of balance, often on a daily basis. Disorders in the balance system is the cause of falls in more than half of the patients aged above 65 years. The prevalence of balance disorders in general has been estimated to be 15% of the population which means that 15% of the population at any given place at any given time will have a balance disorder. Yet then, very few medical centres that includes hospitals and clinics of all sizes be it in the government or in the private sector have requisite modern facilities for rational and scientific management of balance disorders. Diagnosis and treatment of balance disorders have progressed tremendously and medical set-ups everywhere now need to update their health care delivery systems to ensure that balance disorder patients are no longer managed in the way they were treated half a century back.
In the last two decades a huge lot of advancements have taken place in our understanding of the mechanism of balance in the human body, in the diagnostic procedures for identifying disorders in the balance system and of course in the treatment of balance disorders. Modern management of balance disorders is extremely scientific and evidence-based. The age old irrational practice of trying to camouflage the patient’s symptom of head spinning/imbalance by prolonged use of symptom relieving anti- vertigo medicines has now been found to be harmful and deleterious to the subject’s general physical health and especially to the balance system. This practice is hence now denounced and abhorred by the medical community. Vertigo and / or imbalance is just the symptom or manifestation of an underlying medical disorder and is not a disease in itself. The practice of prescribing the anti-vertigo medicines just to provide some symptomatic relief to the patient and to camouflage the spinning sensation was the prevalent practice in the last century as our understanding of the physiology of the maintenance of balance was not very clear and diagnosis of the underlying cause of the vertigo was not possible as dependable diagnostic tests were not available then. That is however not the case today and doctors who are updated and abreast of the recent advancements in medical science especially in the management of balance disorders can easily diagnose the cause of the balance disorder and offer specific therapy to treat the underlying medical disorder very effectively. The management of balance disorders is now a special branch of medical science called neurotology and doctors who specialise in the management of balance disorders are called neurotologists.
Management of a medical disorder includes two aspects (1) diagnosis, and (2) treatment. Though in medical parlance vertigo/unsteadiness/dizziness are completely different entities, in colloquial language the terms are used synonymously. These terms are interchangeably used to convey a huge range of sensations like head spinning, a feeling of rotation of the visual surroundings or a feeling of spinning of objects surrounding the subject, a sensation of spinning inside the head and not of the surroundings, unsteadiness or imbalance, a feeling of wobbling or swaying as if the subject is standing on the deck of a ship and even a loss of spatial orientation. The last term ‘loss of spatial orientation’ is a bit complex and is a medical term to denote loss of orientation of the physical surroundings wherein the subject feels completely disoriented about the immediate physical environment of the place where the subject is located. Each one of these sensations are extremely traumatic to the subject not only physically but also mentally and most, (but not all) of these feelings originate from a disorder in the vestibular system. Not uncommonly patients suffering from a sinking sensation, a feeling of impending faint, blackouts, and even panic attacks (which is a sudden surge in anxiety and fear often with thumping of the chest and breathlessness/ suffocation) also present to the doctor using the term ‘vertigo’ to describe their symptom though none of them are disorders of the balance system. Many psychological disorders like panic attacks, mental depression, feeling of insecurity present to the doctor with the complain of unsteadiness/vertigo. The clinician must be astute and discerning enough to be able to identify whether the patient is actually having a disorder in the balance system or is it something else like a low blood pressure, generalised weakness, anaemia, or some psychological disorder.
The term ‘vertigo’ is not the name of any disease, it is just the English translation of ‘chakkar’ or ‘matha ghora’ just as fever is the English translation of ‘bukhar’ or ‘jor’. ‘Vertigo’ is a term which the patient is expected to tell the doctor; if the doctor tells the patient that the patient has ’vertigo’, it means that the doctor has merely acted as a translator and has not done his job as a doctor. If a doctor makes a diagnosis of ‘vertigo’, it merely means that the doctor has not been able to find out the cause and has used the term ‘vertigo’ to camouflage his/ her ignorance. As the healthcare provider, the doctor’s job is to diagnose the cause of the vertigo and treat the underlying disorder that is causing the vertigo. Treating balance disorders with anti-vertigo medications that provide only symptomatic relief is like treating malaria / typhoid/ pneumonia with anti-pyretics like paracetamol. They may at best temporarily supress the symptom but will in no way correct the disease.
Diagnosis:
Diagnosis in vertigo requires a (1) a very very detailed history taking with complete description of each event, (2) some clinical tests and (3) some investigations. The most important of these three is a very detailed history with emphasis on the word ‘very’. This history taking is a pretty time consuming tedious affair and though a detailed history is the key to diagnosis for many medical disorders, it is nowhere more important than when trying to diagnose a patient of vertigo. Even if a clinic has the best of modern investigative facilities for a vertigo patient, yet without a proper history and description of the patient’s symptoms, it is impossible to make a correct diagnosis. Time is the biggest constraint in doing justice to a patient of vertigo as not only does the history taking and a detailed description of complaints take a huge lot of time and patience /perseverance on the part of the doctor, most of the investigations related to vertigo also requires quite a lot of time and also specially trained personnel. These are the main reasons why most medical establishments do not afford to run vertigo clinics as spending so much time on one patient is not economically viable in most medical setups and also most patients now a days are always on the go (if not on the run) and want quick-fix solutions for their ailments.
The clinical tests involve a complete evaluation of the general condition of the patient, carrying out some basic neurological tests, basic hearing tests and a very detailed clinical evaluation of the balance system.
Investigations in a patient of vertigo comprise of tests to evaluate the structural and functional integrity of the balance system. As already mentioned, a huge lot of advancement has taken place in the diagnostic tests and today the diagnostic armamentarium of the neurotologist has sharpened so much that any disorder in the balance system can be diagnosed with utmost precision and with pinpoint accuracy. The diagnostic tests that are carried out to evaluate the balance system are called the vestibular function tests (VFT) and the discipline is called vestibulometry. Our understanding of vestibular physiology and mechanism of maintenance of balance in the human body has undergone a sea change in the last decade. Today we know the exact function of each part of the balance system. With the recent advancements in vestibulometry, any lesion in the vestibular system can be very precisely and accurately diagnosed provided all the vestibular function tests are properly done. Neurologists who are updated with the knowledge/ expertise/ instrumentation of contemporary diagnostic modalities can localise the site of lesion in nearly all cases and find out the causative disease in most if not all cases. Topographic and etiologic diagnosis is a REALITY today in most cases presenting with balance disorders. Each and every part of the vestibular labyrinth – the 3 semi-circular canals, the utricle and the saccule, the sup vestibular nerve and the inferior vestibular nerve can be individually tested and its functional status ascertained accurately. Each part of the balance system has a different function and needs to be evaluated separately.
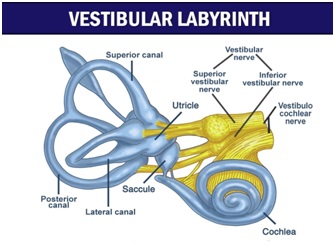 The balance organ situated deep inside the ear, one on each side is called the vestibular labyrinth and each houses five different sensors to sense different types of movement. The saccule senses up-down movement in the vertical axis e.g., when we are going up or down in a lift, the utricle senses linear movement in the horizontal plane i.e., front back and side to side movement e.g., when we walking are moving in a walkalator and the three semi-circular canals sense movement in different angular planes like rotating the head side to side (when we gesture ‘no’ or when we turn our head to the left / right side is sensed by the lateral semi-circular canals, gesturing ‘yes’ i.e., moving the head up-down or looking up e.g., when we try to look at the ceiling or to the ground is sensed by the anterior / posterior canals). In all our day to day activities, these sensors are used every moment of our lives. When we put our head down to sip a cup of tea we are using the anterior canals and when we put the head up after sipping the tea we use our posterior canals. When I bend down to tie the shoe laces of my right leg the movement is sensed by the right anterior semi-circular canal. All these sensors work in unison and in harmony to sense any movement/ destabilisation of the body. Any movement of the head or of the body however small or big must be sensed very accurately by the sensors of the vestibular / balance system for the brain to maintain balance. The maintenance of balance is an ongoing dynamic process. Every moment of our lives we use all these sensors to maintain our body’s position and also to visualise the physical surroundings. A defect in any one of the sensors can jeopardise the balance system completely and lead to unsteadiness (imbalance) and /or head spinning (vertigo). Modern vestibulometry allows us to test each part separately. The sensors of the vestibular labyrinth after sensing the movement sends the information to the brain which then brings about corrective measures in the form of contraction of different muscles in the body to maintain our erect posture and a sense of visual stability of the surroundings. If the former is improper we feel unsteady and if the latter is improper we feel head spinning. The visual inputs from the eyes which sense the stability of the surroundings and some inputs from special sensors in different parts of the body like that in the soles of the foot that sense the stability of the ground supplements the information from the vestibular labyrinths and helps the brain to execute the right and the most suitable corrective action. The body is continually being destabilised as our physical surroundings are moving and we are also moving and it due to the relentless and continuous activity of the balance system which is persistently generating the requisite corrective action that we are not being destabilised and the surroundings are appearing stable to us.The above is of course an over-simplification of a very complex biological system in the human body and it takes a medical person specialised in neurotology to get an insight into the very complex working of the balance system and to detect any derangements in its functioning. Different parts of the brain play a very important part in shaping the nature of the corrective action executed by the brain. A proper treatment is possible only after the disorder has been accurately diagnosed. The mechanism of maintenance of balance is the most complex of all the biological systems of the human body and involves the harmonious functioning of different organs like the brain/eyes/ nerves/ muscles/ some special sensors in the vestibular system like the ones mentioned above and many biological systems like the nervous system, the musculo-skeletal system, the vestibular system and even the cognitive and psychic systems. Hence diagnosing disorders of the balance system and treating them scientifically and logically involves quite an effort and requires a high degree of expertise and sophistication. Only specialised centres with requisite infrastructure in the form of man and machine can do justice to managing patients having disorders in the balance system.
The balance organ situated deep inside the ear, one on each side is called the vestibular labyrinth and each houses five different sensors to sense different types of movement. The saccule senses up-down movement in the vertical axis e.g., when we are going up or down in a lift, the utricle senses linear movement in the horizontal plane i.e., front back and side to side movement e.g., when we walking are moving in a walkalator and the three semi-circular canals sense movement in different angular planes like rotating the head side to side (when we gesture ‘no’ or when we turn our head to the left / right side is sensed by the lateral semi-circular canals, gesturing ‘yes’ i.e., moving the head up-down or looking up e.g., when we try to look at the ceiling or to the ground is sensed by the anterior / posterior canals). In all our day to day activities, these sensors are used every moment of our lives. When we put our head down to sip a cup of tea we are using the anterior canals and when we put the head up after sipping the tea we use our posterior canals. When I bend down to tie the shoe laces of my right leg the movement is sensed by the right anterior semi-circular canal. All these sensors work in unison and in harmony to sense any movement/ destabilisation of the body. Any movement of the head or of the body however small or big must be sensed very accurately by the sensors of the vestibular / balance system for the brain to maintain balance. The maintenance of balance is an ongoing dynamic process. Every moment of our lives we use all these sensors to maintain our body’s position and also to visualise the physical surroundings. A defect in any one of the sensors can jeopardise the balance system completely and lead to unsteadiness (imbalance) and /or head spinning (vertigo). Modern vestibulometry allows us to test each part separately. The sensors of the vestibular labyrinth after sensing the movement sends the information to the brain which then brings about corrective measures in the form of contraction of different muscles in the body to maintain our erect posture and a sense of visual stability of the surroundings. If the former is improper we feel unsteady and if the latter is improper we feel head spinning. The visual inputs from the eyes which sense the stability of the surroundings and some inputs from special sensors in different parts of the body like that in the soles of the foot that sense the stability of the ground supplements the information from the vestibular labyrinths and helps the brain to execute the right and the most suitable corrective action. The body is continually being destabilised as our physical surroundings are moving and we are also moving and it due to the relentless and continuous activity of the balance system which is persistently generating the requisite corrective action that we are not being destabilised and the surroundings are appearing stable to us.The above is of course an over-simplification of a very complex biological system in the human body and it takes a medical person specialised in neurotology to get an insight into the very complex working of the balance system and to detect any derangements in its functioning. Different parts of the brain play a very important part in shaping the nature of the corrective action executed by the brain. A proper treatment is possible only after the disorder has been accurately diagnosed. The mechanism of maintenance of balance is the most complex of all the biological systems of the human body and involves the harmonious functioning of different organs like the brain/eyes/ nerves/ muscles/ some special sensors in the vestibular system like the ones mentioned above and many biological systems like the nervous system, the musculo-skeletal system, the vestibular system and even the cognitive and psychic systems. Hence diagnosing disorders of the balance system and treating them scientifically and logically involves quite an effort and requires a high degree of expertise and sophistication. Only specialised centres with requisite infrastructure in the form of man and machine can do justice to managing patients having disorders in the balance system.
Investigations in a vestibular disorder patient as available today are video-nystagmography (VNG), the ocular and cervical vestibular evoked myogenic potentials (oVEMP and cVEMP), Dynamic Visual Acuity test (DVA), the Video Head Impulse Test (VHIT), Subjective Visual Vertical test (SVV), Craniocorpography (CCG), posturography, some audiological (or hearing) tests like Audiometry, Electrocochleography (ECochG) and Brainstem Evoked Response Audiometry (BERA). Each of these tests evaluate a specific portion of the balance system and none is a replacement of the other. The audiological tests though not literally a part of vestibulometry are yet important as in many disorders of the balance system the hearing also gets affected and hearing tests present some peculiar and typical patterns in some specific types of balance disorders that help in diagnosis of the balance disorder. Though commonly carried out, yet imaging studies like CT scan or an MRI of the brain are usually not that effective as a diagnostic tool in most cases of head spinning, but are very important in patients presenting with instability/unsteadiness.
Treatment:
Unfortunately however, though balance disorders are so very common, very few hospitals and clinics have the requisite setup for doing justice to balance disorder patients. No wonder whenever a patient visits a doctor with a balance disorder, mostly the diagnosis is made as ‘vertigo’ and the treatment offered is a mix of anti-vertigo drugs to camouflage the symptom of vertigo. Both are equally deplorable and illogical.
Treatment has to in accordance to the cause of the vertigo/imbalance if any. Not uncommonly though the patient presents with the complain of vertigo there is actually no disorder whatsoever in the balance system. It is now known that about 40% of patients who report to the doctor with vertigo/imbalance do not have any disorder in the balance system at all. Many of these patients actually have conditions like neuro-cardiogenic syncope, orthostatic hypotension, generalised weakness due to metabolic disorders (like diabetes, thyroid disorders, anaemia) or even panic attacks and other types of psychological disorders. None of these have any relationship at all with the balance system. A thorough history taking and asking leading questions usually helps in identifying these disorders; sometimes some investigations may be required for confirmation. Usually, but not always these patients present with symptoms of a sinking sensation, blurring of vision, blackouts, features of anxiety, impending faint, fear of falls etc. An astute clinician does not have much problems in sieving out these conditions provided he has been able to spend adequate time in eliciting the history properly. These patients do not have any disorder in the balance system but if they are mis-diagnosed as a balance system disorder and persistently treated with the vestibular sedatives/anti-vertigo drugs they induce an actual balance disorder by sedating and /or jeopardising a perfectly functioning vestibular system.
If however the patient is suspected to have a disorder in the balance system, then of course the requisite detailed history taking, clinical tests and requisite investigations are mandated to arrive at a definitive diagnosis. Neurotology today is an evidence based medical discipline and treatment is directed to any documentable evidence of abnormality and any arbitrary or empirical medication is irresponsible and unethical on the part of the doctor.
The commonest cause of head spinning for which a patient presents to the doctor is a condition called positional vertigo. Such patients commonly present with recurrent head spinning for a few seconds only on change of head posture; they feel an abrupt head spinning often pretty severe whenever they try to get up from bed or lie down in bed, turn towards one side, try to look up towards the ceiling or bend down to pick up something from the floor Usually it is a benign harmless self-limiting condition that needs to be corrected by some physical manoeuvres carried out by a trained professional i.e., a doctor who is trained in handling such patients. There is no valid medical treatment for these conditions and treating such patients with anti-vertigo drugs is illogical, unscientific and deplorable. It implies that the treating doctor has not been able to identify the cause of the disorder and/or does not have the expertise to carry out the requisite physical manoeuvre.
Most of the other causes of vertigo/imbalance can be diagnosed pretty easily provided the clinician has been able to elicit and extract the detailed history from the patient, has carried out the requisite clinical tests and the required investigations of the balance system (vestibular function tests/ vestibulometry, imaging studies etc.). Treatment is usually in the form of medication and physical therapy. The common causes of balance disorders after positional vertigo are e.g., Vertiginous migraine, vestibular neuritis, labyrinthitis, Ménière’s disease, disorders in the brain like vestibular epilepsy, vestibular paroxysmia, tumours and strokes in the brain, degenerative changes in the nerves like since the ataxia etc. For each specific disorder, specific treatment protocols are available which if judiciously used controls/cures the medical abnormality that is causing the vertigo or imbalance. Balance disorders can be due to a wide variety of causes, ranging from disorders in the ear to that in the brain, to that of the nervous system as well as that of the eyes. Diagnosis and treatment of balance disorders have advanced so very much in the last few years that not being able to diagnose the underlying disease that is causing a balance disorder and inability in treating it no longer acceptable. Many of the commonly prescribed anti-vertigo drugs are not approved in Western countries like the US and even when used in places where they are available like in India, the current medical consensus is to restrict the use to a maximum of 3-5 days never beyond that. Actually if the clinician has been able to identify the underlying causative disorder he does not need to prescribe these vestibular sedatives/ anti-vertigo drugs. These drugs are all potentially harmful and are prescribed only when the clinician has not been able to identify the causative disorder.
Treatment of balance disorders does not mean containing the causative disease only by prescribing medicines to treat the disorder like prescribing diuretics for Meniere’s disease or prescribing migraine prophylactic medications for vertiginous Migraine. It also involves restoring the balance function which has been damaged by disease. This is possible by physical therapy only. Nowadays, a lot of advancements have been made in the physical therapy for balance disorder patients and specific physical therapy to stimulate specific parts of the vestibular labyrinth are now available. Since the vestibulometric tests can precisely localise the defective organ in the balance system, specific physical therapy to stimulate the functional status of the defective organ is now possible. Tai-chi and Yoga have been found to be very effective in improving balance function and are slowly replacing the age-old Cawthrone-Cooksey exercises. The later has been converted into a joke by doctor’s doling out some tear-away sheets printed by some pharma companies with names of some anti-vertigo medicine advertised there and handing them over to patients expecting that patients will be able to carry out the exercises properly. These exercises, including the Cawthrone-Cooksey Excersises need to be taught and demonstrated by trained and qualified physical therapists and experts in yoga and tai chi. . In keeping with the advancements in diagnostic neurotology, therapeutic neurotology especially physical therapy has also undergone great sophistication. Specific physical therapy to stimulate the functional status of the defective sense-organ is now possible after modern vestibulometry has identified the defective organ in the vestibular labyrinth or in other parts of the balance system. Experts in physical therapy for balance disorder patients and specialists in neuro rehabilitation work in coordination with neurotologists to provide a much better quality of life to most if not all balance disorder patients. A huge lot of electromechanical gadgetry is now available for this and modern technology like virtual reality is being used to restore normalcy to the deranged balance function. The results of such physical therapy is extremely promising.